Question: Is it worth taking Osteoporosis medications considering the side effect risks?
What is Osteoporosis?
As a result of declining hormones, the bone mineral density declines. This causes a brittle and fragile bone from a deficiency in calcium and vitamin D. The spectrum of breakdown can be gradual decline from normal bone moving to osteopenia and then to osteoporosis.
Osteopenia is defined by a reduced bone mass much like osteoporosis however it has not reached the severity of decreasing bone mineral density.
How do you get Osteoporosis?
Without blaming age… In the medical world we see bone density decline for several reasons. The fundamental pathology is essentially the same regardless of age. There is essentially a decline in estradiol (hormone) that leads to an increase imbalance between osteoclast vs. osteoblast activity.
Osteoclasts are the cells that chew up old bone and resorb it. Osteoblasts are the cells that lay down new bone. If there is an event that increases osteoclastic activity, the density will decline. Think about having more mouths to feed but only so much bone to go around. On the flip side, you could also have an event that suppresses osteoblastic activity. This means the normal amount of osteoclasts are functioning but you just don’t have the fuel to fire up the osteoblasts.
The Root Cause
It is important to understand the root cause of your osteoporosis before selecting a treatment. If your diet is crap and you never see the sun, chances are you have a nutritional deficiency. Therefore, fixing your nutritional imbalance will go a long way in increasing your bone density. If you are post-menopausal or no longer having a “period” you would be considered “anovulatory”.
Anovulatory means you no longer pop out an egg every month. That egg you once ovulated was responsible for releasing that important estradiol that limited osteoclastic activity. The basic oversimplification remains fairly complicated. I will do my best to explain.
Estradiol is like a defensive line against the RANKL protein. RANKL is trying to connect the osteoclast to the bone. If estradiol is able to block it from the oncoming osteoclasts, the bone remains safe and the Osteoblasts can do their thing.
Types of Treatment
As of this writing there are a few basic treatments that your question is alluding to.
- Menopausal Hormone Therapy (MHT)
- It makes sense that if you are anovulatory and lacking estrogen you should replace it. In 2017 the United States Preventative Service Task Force (USPSTF) published updated information in the Journal of the American Medical Association. The findings indicated that a combined estrogen/progestin replacement therapy had minimal benefit in preventing chronic conditions in post menopausal women. The USPSTF also went on to say Estrogen alone had “no net benefit for the primary prevention of chronic conditions for most postmenopausal women who have had a hysterectomy.”
- The official statement from the USPSTF as of November 1st 2022 recommends against the use of estrogen/progestin combo for primary prevention and against the use of estrogen alone for the same in postmenopausal women with a hysterectomy.
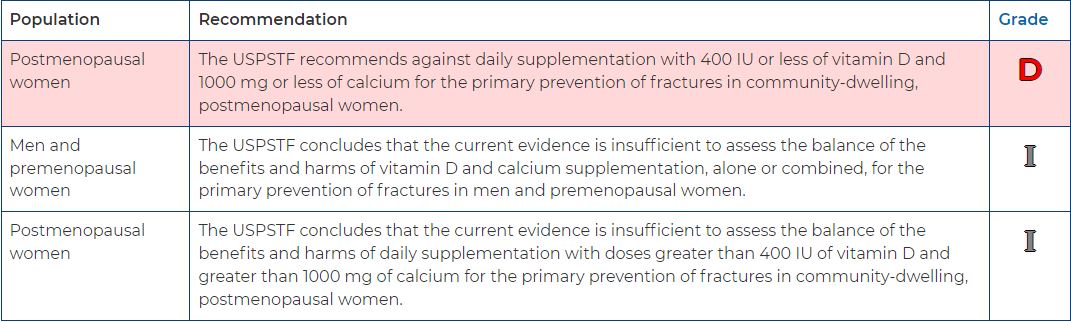
- Calcium and Vitamin D supplements: USPSTF recommended in 2018 but is actively being revised and updated.
- Antibody based treatments like Denosumab
- An “mab” type medication is a Monoclonal AntiBody. The antibody is again a defensive line. It will grab onto the RANKL protein and prevent it from hooking up with the osteoclast. The osteoclast is then unable to actively chew up the bone.
- in 2020 Ning Zhang et. al. published their findings and commented on the abundance of RANKL throughout other systems in the body. Side effects are based on the non-selective binding and essentially stopping numerous other processes in the immune system. The side effects were rare and noted to be fairly close to the placebo group. They noted a 1.7% risk of osteonecrosis of the jaw.
- Bisphosphonates (alendronate, riserdronate, ibandronate)
- These medications get eaten up by the osteoclasts. Once inside the osteoclast they inhibit a chemical process that is not worth detailing here so lets just call it FPPS. This creates a number of effects inside the osteoclasts but ultimately results in the osteoclasts untimely demise.
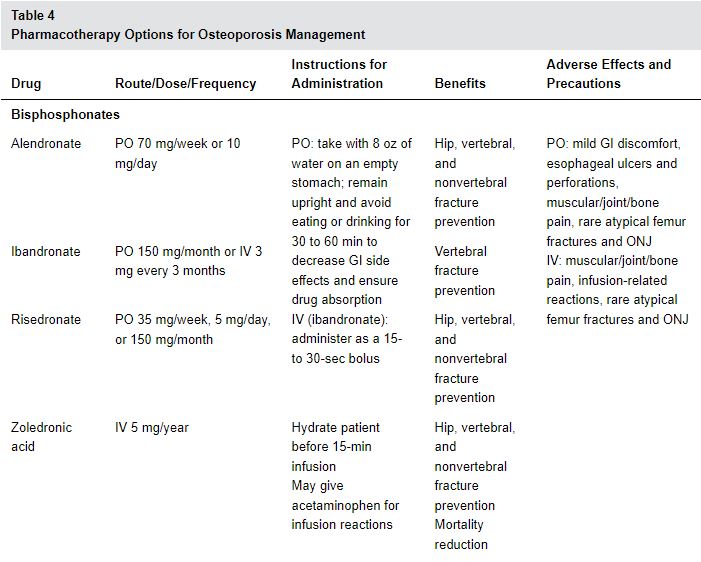
- The American Academy of Family Physicians (AAFP) published an amazing table outlining these drugs with their adverse effects.
What Does The Evidence Show?
The consensus so far is a “definitely maybe” and only acts to confound the scenario. The risk of any treatment is based on individual circumstances. However, there have been some decent studies that put it into perspective for us. Specifically, in June 2021, J. Brown published a study on “Long Term Treatment of Postmenopausal Osteoporosis” in the Endocrinology and Metabolism journal. The article had a figure that compared treatment groups to non-treatment groups specifically looking at fractures related to osteoporosis.
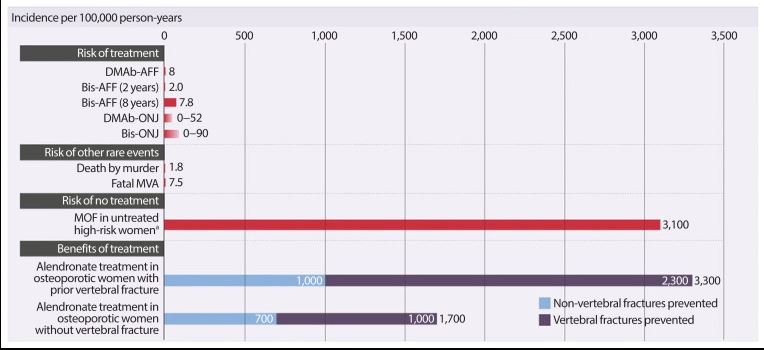
This figure shows DMAb-AFF (Denosumab associated atypical femur fracture), Bis-AFF (Bisphosphonate associated atypical femur fractures), DMAb-ONJ (Denosumab associated osteonecrosis of the jaw) and finally Bis-ONJ which I assume you get the point of what that one means.
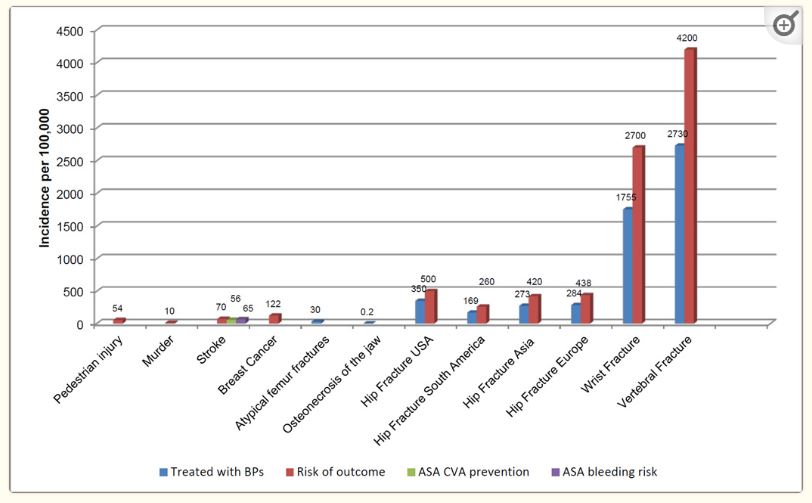
Clearly the risk of Major Osteoporotic Fractures (MOF) is higher in an untreated population. This data is remarkably similar to another study published back in 2016 by Adler et. al., showing the following figure that may be easier to read.
Why are Hormones Bad Again?
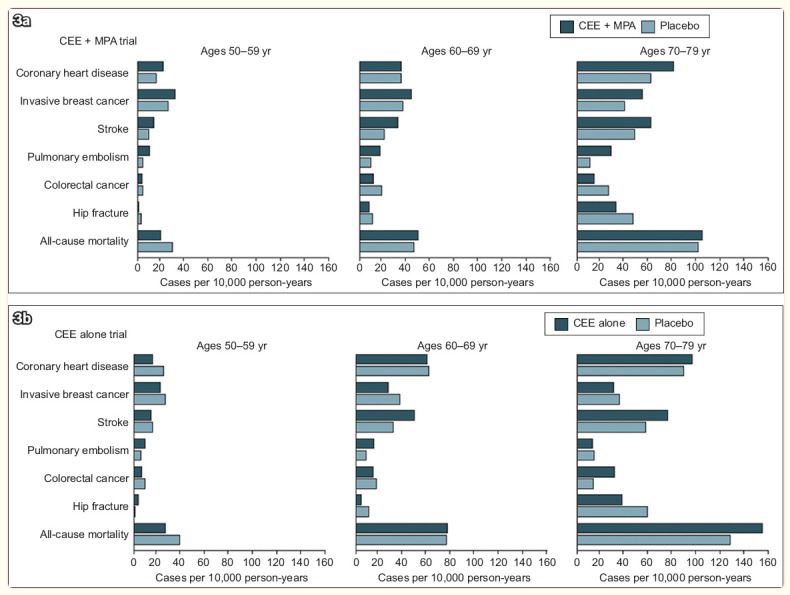
CEE: Conjugated equine estrogens (estrogen)
MPA: Medroxyprogesterone acetate (Progesterone)
This graph is originally from a JAMA article published in 2013. This shows the increased risk of heart disease, stroke, breast cancer and blood clots vs. placebo. The scary part is that the older the study population got the higher the risks were of adverse outcomes were. It reminds me of a study I once saw that showed a linear correlation that “mortality increases with age”. To drive that point home thats like saying the older you get, the more likely you are to die… Thanks for wasting research dollars on the obvious, but I digress.
The Bottom Line
Is it worth taking medications to treat osteoporosis? The Endocrine society, AAFP, USPSTF, and numerous other entities suggest it is. The risks associated treatment is completely based on a number of factors that would likely be unique to your specific scenario. Treatment modalities should be evaluated regularly to make adjustments. There is no straight answer to this one other than stating “definitely maybe” and directing you to discuss with your health care professional.



Very thorough and informative, thank you!